small intestinal bacterial overgrowth
- related: GI
- tags: #GI
Small Intestinal Bacterial Overgrowth
This patient has bloating, flatulence, diarrhea, and macrocytic anemia, which, given her history of Roux-en-Y gastric bypass, should raise suspicion for small intestinal bacterial overgrowth (SIBO).
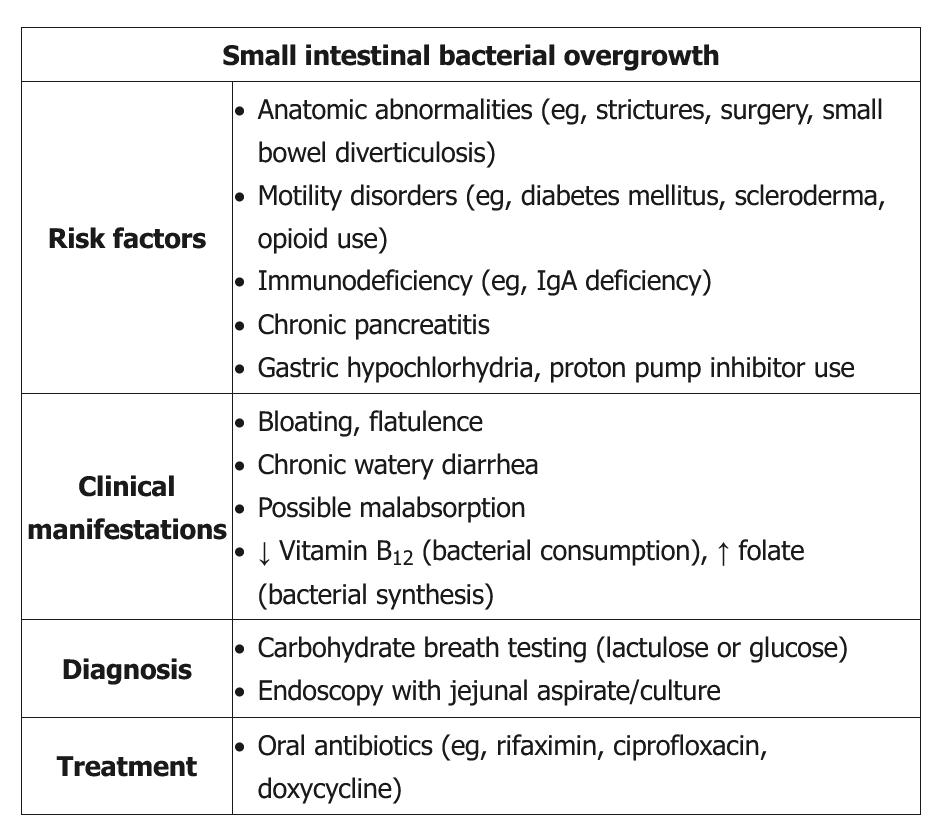
SIBO is common in patients who have undergone gastrointestinal bypass surgery as the procedure forms a blind loop of intestine, allowing for excessive bacterial growth. SIBO usually presents with abdominal distension and discomfort, flatulence, and diarrhea. Severe or prolonged disease can cause fat malabsorption leading to steatorrhea, weight loss, and nutritional deficiencies (ie, vitamins A, D, B1, B12). Macrocytic anemia from vitamin B12 deficiency is a common laboratory finding.
The diagnosis of SIBO is made with a positive hydrogen breath test or jejunal aspiration and culture with high levels of bacterial colonization. Most patients are treated with antibiotics (eg, rifaximin). Recurrence is common and is typically treated with a second course of antibiotics.
Irritable bowel syndrome is characterized by chronic abdominal pain that improves with bowel movements, altered bowel habits, and a feeling of incomplete evacuation. Anemia and nutritional deficiencies suggest an alternate diagnosis.
Microscopic colitis causes diarrhea and pain, but patients are generally older (age ≥50) and typically develop watery diarrhea (5-10 episodes per day) rather than large, bulky stools and flatulence. In addition, inflammatory markers are elevated in ≥50% of patients.
Small intestinal bacterial overgrowth (SIBO) is caused by various conditions, including impaired motility, strictures (for example, in Crohn disease), or blind loops (for example, small-bowel diverticula). There is some evidence that SIBO could contribute to symptoms in IBS-D.
Classically, SIBO is defined by the presence of more than 105 colony-forming units per mL of jejunal aspirate. Based on its use in research studies, jejunal aspirate is considered the gold standard but is often not used in clinical practice due to the requirement for endoscopy to obtain cultures, the patchy nature of small intestinal overgrowth, and oropharyngeal contamination of the specimen. Glucose and lactulose breath tests have acceptable specificity (around 80%) but poor sensitivity (30%-40%) for diagnosing SIBO. Diagnosis requires typical symptoms and a confirmatory test (usually breath testing), although empiric antibody therapy with monitoring for improvement in symptoms may be reasonable in patients with a high probability of SIBO. Treatment consists of antibiotic therapy and often requires repeated courses if the underlying condition cannot be resolved.
This patient has symptoms consistent with diabetic diarrhea; a painless, watery diarrhea that can occur at night and is often associated with fecal incontinence. Patients may have periods of normal bowel movements and/or constipation. The etiology is likely multifactorial but is thought to be largely due to autonomic neuropathy leading to small bowel and colonic hypomotility, increased intestinal fluid secretion, and anorectal dysfunction. Diabetic diarrhea is a diagnosis of exclusion; workup includes stool studies, serum chemistries and endocrine studies, and endoscopic biopsy.
Small intestinal bacterial overgrowth (SIBO) commonly contributes to diabetic diarrhea as gastrointestinal hypomotility allows for excessive colonization. This leads to abdominal discomfort, bloating, and flatulence; severe disease can cause malabsorption with steatorrhea and vitamin deficiency. Patients with bacterial overgrowth often have secondary lactose intolerance as well. The diagnosis of SIBO can be confirmed with a carbohydrate breath test and treated with antibiotics (eg, rifaximin); endoscopic and histopathologic studies are often nonrevealing. Patients with diabetic diarrhea in the absence of SIBO are often treated with antimotility agents (eg, loperamide).